
Popular topics

-
References
Adegbola SO et al. (2018). Anti-TNF therapy in Crohn’s disease. Int J Mol Sci 19, 2,244.
Banerjee R et al. (2020). Biologics for the management of inflammatory bowel disease: a review in tuberculosis-endemic countries. Gut Liver 14, 685-698.
Bosca-Watts MM et al. (2015). Pathogenesis of Crohn’s disease: Bug or no bug. World J Gastrointest Pathophysiol 6, 1-12.
Cai Z et al. (2021). Treatment of inflammatory bowel disease: a comprehensive review. Front Med (Lausanne) 8, 765474.
Cherry LN et al. (2015). Vedolizumab: an α4β7 integrin antagonist for ulcerative colitis and Crohn’s disease. Ther Adv Chronic Dis 6, 224-233.
Fragoulis GE et al. (2019). JAK-inhibitors. New players in the field of immune-mediated diseases, beyond rheumatoid arthritis. Rheumatology (Oxford) 58, i43-i54.
Friedberg S et al. (2023). Upadacitinib Is effective and safe in both ulcerative colitis and Crohn’s disease: prospective real-world experience. Clin Gastroenterol Hepatol 21, 1,913-1,923.
Ha C and Kornbluth A. (2014). Vedolizumab as a treatment for Crohn’s disease and ulcerative colitis. Gastroenterol Hepatol (NY) 10, 793-800.
Hu X et al. (2021). The JAK/STAT signaling pathway: from bench to clinic. Signal Transduct Target Ther 6, 402.
Humphry N. (2022). Safety of anti-TNFs in patients with immune-mediated disease. EMJ Gastroenterol. Accessed 09.29.23.
Loftus Jr ED et al. (2023). Upadacitinib induction and maintenance therapy for Crohn's disease. N Engl J Med 388, 1966-1980.
Schwartz DM et al. (2018). JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat Rev Drug Discov 17, 78.
Shepard HM et al. (2017). Developments in therapy with monoclonal antibodies and related proteins. Clin Med (Lond) 17, 220-230.
Slevin SM and Egan LJ. (2015). New insights into the mechanisms of action of anti-tumor necrosis factor-α monoclonal antibodies in inflammatory bowel disease. Inflamm Bowel Dis 21, 2,909-2,920.
World Health Organization, Biologicals: https://www.who.int/health-topics/biologicals#tab=tab_1. Accessed 09.23.23
Zheng Y et al. (2014). TNFα promotes Th17 cell differentiation through IL-6 and IL-1β produced by monocytes in rheumatoid arthritis. J Immunol Res 2014, 385382.
No Guts, No Glory: Innovative Treatments for Crohn’s Disease
Crohn’s disease (CD) is a type of inflammatory bowel disease (IBD) characterized by chronic inflammation of the gastrointestinal (GI) tract. A common theory regarding the mechanism of CD accuses typically harmless bacteria in the gut microbiome of being the culprit behind triggering the excessive and inappropriate immune response. Immune cells overreact and undertake their self-destructive path toward progressive bowel damage, leading to persistent pain and discomfort for those affected (Bosca-Watts et al. 2015).
While there is currently no cure for CD, various treatment options exist to manage inflammation and provide some much needed respite from symptoms of the disease. As with many inflammatory disorders, steroids are often used as the first-line therapy due to their potent anti-inflammatory effects. Unfortunately, steroids are ineffective in around 20% of CD patients and over 20% become steroid-dependent. In this case, biologics or immunomodulators are the next option (Banerjee et al. 2020).
In this blog, we will discuss the different methods utilized to treat CD, including the more commonly used biologics and the newly approved Janus kinase (JAK) inhibitor, upadacitinib.
Dam the Cytokine Flow
Let’s start by discussing biologics. Simply put, biologics are a class of drug that are derived from living culture systems, including bacteria, yeast, or mammalian cells. One class of biologic that has become increasingly important in the treatment of chronic inflammatory diseases is monoclonal antibodies (mAbs). In particular, mAbs which block tumor necrosis factor (TNF) have become the most broadly utilized for autoimmune and inflammatory conditions (Shepard et al. 2017). TNF is a remarkably good target in these settings as it sits at the apex of a cascade of pro-inflammatory cytokines, so the blockade of TNF not only disrupts TNF signaling itself but also inhibits the production and release of various downstream cytokines implicated in the pathogenesis of these diseases, such as IL-1β and IL-6 (Zheng et al. 2014).
With this in mind, it’s not surprising that TNF inhibitors are commonly used in the treatment of CD. In fact, there are multiple anti-TNF mAbs currently approved for the treatment of CD; infliximab (Remicade), adalimumab (Humira), and certolizumab pegol (Cimzio), as well as several biosimilars to Remicade and Humira (Adegbola et al. 2018). Infliximab and adalimumab are full mAbs, both with human Fc regions (the region that can interact with receptors on the cell surface) and with mouse and human antigen-binding regions (known as fragment antigen-binding or Fab), respectively. Certolizumab pegol, on the other hand, is not a full antibody, instead it consists of a humanized Fab fragment conjugated to polyethylene glycol, which serves to increase the half life and solubility of the molecule in vivo.
Despite their differences in structure, all these mAbs function by binding to soluble TNF, and to a lesser extent transmembrane TNF, to block its binding to the TNF receptor, subsequently inhibiting its signaling cascade (Slevin and Egan, 2015).
Unfortunately, up to 40% of patients with IBD do not respond to anti-TNF therapy within the initial treatment period and approximately 20-40% of patients respond initially but progressively lose responsiveness within one year (Cai et al. 2021). Additionally, though anti-TNF therapies are generally well tolerated, there are still potential side effects associated with the treatment, including immunogenicity and an increased susceptibility to infections, most commonly tuberculosis, which can be reactivated from its latent form upon suppression of the immune system (Humphry 2022).
Block the Traffic
Due to the considerable proportion of patients who experience an inadequate response to TNF-blocking mAbs, there was a need for therapies that target alternative pathways involved in CD. This led to the introduction of mAbs targeted against integrins. Integrins are receptors that mediate cell-to-cell and cell-to-extracellular matrix adhesion and are named after the α and β subunits of which they are composed. In CD, integrins expressed on the surface of T cells enable their trafficking into the gut, where they enact their damage.
Natalizumab (Tysabri) is a humanized mAb that targets the α4 integrin subunit, allowing it to block the action of both α4β1 (which binds to VCAM-1) and α4β7 (which binds to MadCAM-1), two integrins associated with cell migration in the gut. While α4β7 has been shown to be specific to gut lymphocytes, α4β1 has also been associated with lymphocyte migration in the central nervous system (CNS). Although this enables the use of natalizumab for the treatment of multiple sclerosis in addition to CD, it unfortunately also increases the risk of a fatal CNS infection instigated by the John Cunningham virus, known as progressive multifocal leukoencephalopathy (PML). As a result of this, the therapeutic use of natalizumab for CD is limited (Ha and Kornbluth, 2014).
Vedolizumab (Entyvio), on the other hand, is a humanized mAb used to treat CD that selectively blocks the gut-specific α4β7, specifically blocking trafficking of lymphocytes into the GI tract, resulting in an efficacious treatment of CD with a significantly improved safety profile compared to natalizumab treatment (Cherry et al. 2015).
HiJAK the Pathway
So far, we have dealt predominantly with biologics for CD treatment. However, other classes of drugs have also been proven to be effective. One of these is upadacitinib (Rinvoq), a small molecule drug that inhibits Janus kinase (JAK) and has recently been approved for the treatment of CD.
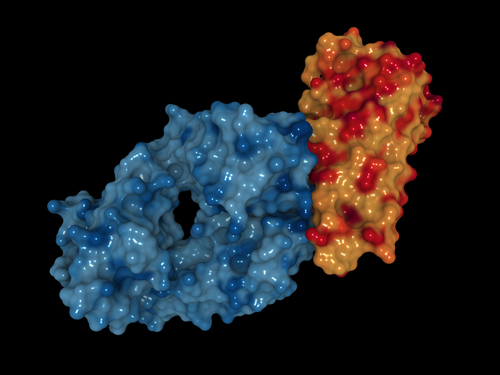
The JAK/signal transducers and activators of transcription (STAT) pathway has been implicated in the pathogenesis of various immune-related diseases, including CD, due to its role in signal transduction of many cytokines (Fragoulis GE 2019). The JAK/STAT pathway works as follows: receptor dimerization is prompted upon cytokine binding, which triggers transphosphorylation of members of the JAK family (consisting of JAK1, JAK2, JAK3, and tyrosine kinase 2 (TYK2) associated with the receptors, causing activation of the JAK molecules and allowing further phosphorylation of the receptors themselves. Phosphorylation of the receptor facilitates the binding of STATs, bringing these molecules into contact with JAKs, which can then also phosphorylate the STATs. Phosphorylated STAT molecules dissociate and form dimers with each other, translocating to the nucleus, and subsequently regulating the transcription of target genes (Figure 1) (Hu et al. 2021).

Fig 1. The JAK/STAT signaling pathway.
First-generation JAK inhibitors were developed to block multiple members of the JAK family, however several side effects, such as infection, anemia, and cardiovascular disease, were associated with their use. Therefore, second-generation JAK inhibitors focused on developing more selective drugs to reduce adverse effects (Schwartz et al. 2018). Upadacitinib has increased selectivity for JAK1, preferentially binding to it, and blocking the phosphorylation and subsequent activation of STATs, hence preventing the flow of the inflammatory cytokine signaling cascade (Friedberg et al. 2023).
Two phase three studies, named U-EXCEED and U-EXCEL, recently demonstrated the efficacy of upadacitinib in CD. Patients with moderate to severe CD were recruited and blindly assigned to receive either oral upadacitinib or placebo once a day for 12 weeks. The Crohn’s Disease Activity Index (CDAI) scores of patients, which takes into account a number of clinical parameters such as body weight, abdominal pain, and number of stools, were used to determine clinical remission and Simple Endoscopic Scores (SES), which are based on the presence and volume of ulcers, the proportion of the surface of the gut covered by ulcers, and the presence and extent of stenosis (narrowing of the intestine), were used to determine the endoscopic response. In U-EXCEL, a significantly higher proportion of CD patients achieved clinical remission compared to placebo treated (49.5% vs 29.1%) and showed an improvement in the endoscopic response (45.5% vs 13.1%). U-EXCEED also showed an overall beneficial response in clinical remission (38.9% vs 21.2%) and endoscopic response (34.6% vs 3.5%) in upadacitinib treated patients compared to placebo treated individuals. An additional study named U-EXCEED showed maintenance of these responses up to 52 weeks after initiation of treatment (Loftus Jr et al. 2023).
Upadacitinib was already approved for use in other immune-mediated disorders, such as rheumatoid arthritis and ulcerative colitis, but is the first JAK inhibitor approved for CD therapy in England and Wales.
Overall, it appears that with the ongoing development of new biologic and small molecule drug therapies targeting the immune system, treatment options for inflammatory conditions such as CD are rapidly expanding. This offers hope of the much sought-after remission to those patients who do not respond, or even lose responsiveness, to currently available medications.
Are You Developing a Biosimilar for Any of These Drugs?
Bio-Rad offers anti-infliximab, anti-adalimumab, anti-certolizumab pegol, anti-natalizumab, and anti-vedolizumab antibodies for the development of highly selective and sensitive pharmacokinetic (PK) and anti-drug antibody (ADA) assays.
References
Adegbola SO et al. (2018). Anti-TNF therapy in Crohn’s disease. Int J Mol Sci 19, 2,244.
Banerjee R et al. (2020). Biologics for the management of inflammatory bowel disease: a review in tuberculosis-endemic countries. Gut Liver 14, 685-698.
Bosca-Watts MM et al. (2015). Pathogenesis of Crohn’s disease: Bug or no bug. World J Gastrointest Pathophysiol 6, 1-12.
Cai Z et al. (2021). Treatment of inflammatory bowel disease: a comprehensive review. Front Med (Lausanne) 8, 765474.
Cherry LN et al. (2015). Vedolizumab: an α4β7 integrin antagonist for ulcerative colitis and Crohn’s disease. Ther Adv Chronic Dis 6, 224-233.
Fragoulis GE et al. (2019). JAK-inhibitors. New players in the field of immune-mediated diseases, beyond rheumatoid arthritis. Rheumatology (Oxford) 58, i43-i54.
Friedberg S et al. (2023). Upadacitinib Is effective and safe in both ulcerative colitis and Crohn’s disease: prospective real-world experience. Clin Gastroenterol Hepatol 21, 1,913-1,923.
Ha C and Kornbluth A. (2014). Vedolizumab as a treatment for Crohn’s disease and ulcerative colitis. Gastroenterol Hepatol (NY) 10, 793-800.
Hu X et al. (2021). The JAK/STAT signaling pathway: from bench to clinic. Signal Transduct Target Ther 6, 402.
Humphry N. (2022). Safety of anti-TNFs in patients with immune-mediated disease. EMJ Gastroenterol. Accessed 09.29.23.
Loftus Jr ED et al. (2023). Upadacitinib induction and maintenance therapy for Crohn's disease. N Engl J Med 388, 1966-1980.
Schwartz DM et al. (2018). JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat Rev Drug Discov 17, 78.
Shepard HM et al. (2017). Developments in therapy with monoclonal antibodies and related proteins. Clin Med (Lond) 17, 220-230.
Slevin SM and Egan LJ. (2015). New insights into the mechanisms of action of anti-tumor necrosis factor-α monoclonal antibodies in inflammatory bowel disease. Inflamm Bowel Dis 21, 2,909-2,920.
World Health Organization, Biologicals: https://www.who.int/health-topics/biologicals#tab=tab_1. Accessed 09.23.23
Zheng Y et al. (2014). TNFα promotes Th17 cell differentiation through IL-6 and IL-1β produced by monocytes in rheumatoid arthritis. J Immunol Res 2014, 385382.
You may also be interested in...

View more Bioanalytical or Immunology blogs















