
Popular topics

-
References
Holloway JW et al. (2010). Genetics of allergic disease. J Allergy Clin Immunol 125, S81-94.
Okada H et al. (2010). The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol 160, 1-9.
Pawankar R (2014). Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J 7, 12.
Wambre E et al. (2017). A phenotypically and functionally distinct human TH2 cell subpopulation is associated with allergic disorders. Sci Transl Med 9, eaam9171.
Th2A Cells — the Latest T Helper Cell Subset and its Role in Allergy
Pollen, ragweed, food, cats, and dust mites are among the most common inducers of severe allergic disorders, which affect approximately 10-40% of the global population (Pawankar 2014). Around 200 to 250 million people suffer from food allergies globally, and 400 million from nasal allergies. Allergies develop as an inappropriate immune response to non-threatening substances, such as pollen. The distinct incidence of allergies in some individuals and not in others has been of significant scientific and general interest. Scientists have postulated that this is linked to genetic predisposition or the lack of early exposure to microorganisms, known as the “hygiene hypothesis” (Okada et al. 2010, Holloway et al. 2010).
A New Subset of T Helper Type 2 Cells
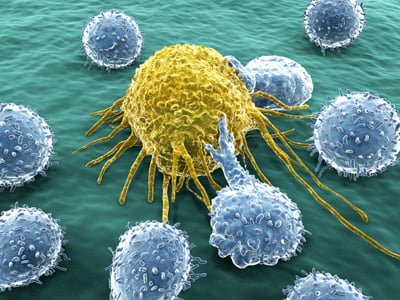
A recent study has added to this scientific exchange with the identification of a unique subset of T helper type 2 (Th2) cells that coordinate allergic responses (Wambre et al. 2017). T helper cells are separate lineages of CD4+ T cells that are involved in coordinating the immune response to pathogens such as bacteria and fungi. There are currently 8 different T helper subsets, and Th2 cells in particular, that are involved in host defense against parasites, as well as the production of IgE antibodies, that react against certain allergens to cause allergic reactions.
Up until now, there was no biological measurement to distinguish between allergy-inducing Th2 cells and those that provide immune protection. Using alder pollen as a model, scientists have finally identified a unique allergic Th2 cell immune signature that characterizes these allergy-inducing cells, naming them Th2A cells (Wambre et al. 2017).
The research team compared allergy restricted CD4+ T cells isolated from the blood of allergic individuals, using pMHC tetramer technology, to the total Th2 cell population. They then performed a fluorescence activated cell sorting screen to assess the cell populations for expression of Th2 specific markers. Both Th2 subsets were defined by their expression of the common Th2 marker CRTH2, which is considered the most reliable marker to identify human Th2 cells.
Compared to the total Th2 cell population, they found that allergy-restricted CD4+ T cells up-regulated their expression of two key molecular markers and down-regulated four others. Accordingly, the newly identified Th2A cells were defined as CRTH2+CD161+CD49d+CD27-CD45RBloCCR7loCD7lo (Wambre et al. 2017).
The research team also confirmed that Th2A cells did not just induce allergies to alder pollen, but were also linked to allergic disorders caused by other allergens including peanut, cat, dust mites, molds such as Aspergillus and Alternaria, as well as timothy grass, which causes seasonal pollen allergies (Wambre et al. 2017).
The clinical relevancy of the Th2A cells was demonstrated in a longitudinal study of peanut-allergic patients completing oral desensitization immunotherapy using an experimental drug with the antigenic profile of peanuts. The study showed that prior to therapy, the vast majority of peanut reactive Th2 cells in these allergic patients demonstrated the Th2A immune signature. Th2A cells were however absent in control non-allergic patients. There was also a significant reduction in the number of Th2A cells in patients who overcame peanut allergy following the treatment (Wambre et al. 2017).
This study has truly challenged and expanded our understanding of T helper subsets. More importantly, it also provides, for the first time, a biological measurement to detect and monitor allergic diseases. Th2A cells can serve as clinical biomarkers to assess the efficacy of allergy treatments. However, further research is needed to determine the mechanisms that drive differentiation of CD4+ T cells into the Th2A subset. This information could lead to the development of strategies to prevent their formation and possibly allergic disorders.
Learn More About Th2 Cells
To learn more about Th2 cells and the other CD4+ T cell subsets, download a copy of our T helper subsets guide which provides an overview of the function of each T helper cell, as well as their biological profile. You can also access antibodies for studying these cells.
References
Holloway JW et al. (2010). Genetics of allergic disease. J Allergy Clin Immunol 125, S81-94.
Okada H et al. (2010). The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol 160, 1-9.
Pawankar R (2014). Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J 7, 12.
Wambre E et al. (2017). A phenotypically and functionally distinct human TH2 cell subpopulation is associated with allergic disorders. Sci Transl Med 9, eaam9171.
You may also be interested in...

View more Immunology or Tips&Tricks blogs















